The Sunday News

Lee-Anne Hall
MENINGITIS is an illness that can lead to paralysis. If misdiagnosed or treated late it can cause disability or even death. There are many types of meningitis but today I would like to speak about the most common one which is bacterial meningitis.
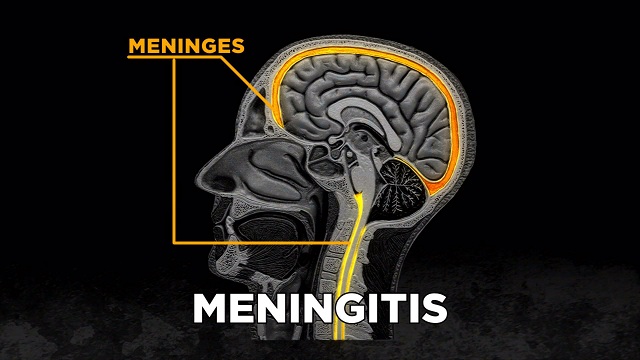
Meningitis is a disease caused by inflammation of the protective membranes covering the brain and spinal cord known as the meninges. The inflammation is usually caused by an infection of the fluid surrounding the brain and the spinal cord.
Meningitis may develop in response to a number of causes, usually bacteria or viruses, but it can also be caused by physical injury, cancer or certain drugs.
The severity of the illness and the treatment is totally dependent on its cause. Thus, it is vital to know the specific cause of meningitis.
Bacterial meningitis is usually severe. While most people with meningitis recover, it can cause serious complications, such as brain damage, hearing loss, or learning disabilities. There are several pathogens (types of germs) that can cause bacterial meningitis.
Risk factors
Factors that can increase your risk of bacterial meningitis include: Age: Infants are at higher risk for bacterial meningitis than people in other age groups. However, people of any age are at risk.
Community setting: Infectious diseases tend to spread more quickly where larger groups of people gather together.
College freshmen living in residence halls and military personnel are at increased risk for meningococcal meningitis.
Certain medical conditions: There are certain diseases, medications, and surgical procedures that may weaken the immune system or increase risk of meningitis in other ways.
Working with meningitis-causing pathogens: Microbiologists who are routinely exposed to meningitis-causing pathogens are at increased risk.
Travel: Travellers to the meningitis belt in sub-Saharan Africa may be at risk for meningococcal meningitis, particularly during the dry season.
Transmission
The germs that cause bacterial meningitis can be contagious. Some bacteria can spread through the exchange (eg, by kissing) of respiratory and throat secretions (eg, saliva or mucus).
Fortunately, most of the bacteria that cause meningitis are not as contagious as viruses that cause the common cold or the flu.
Also, the bacteria are not spread by casual contact or by simply breathing the air where a person with meningitis has been. Other meningitis-causing bacteria are not spread person-to-person, but can cause disease because the person has certain risk factors (such as a weak immune system or head trauma).
Unlike other bacterial causes of meningitis, you can get Listeria monocytogenes by eating contaminated food.
Sometimes the bacteria that cause meningitis spread to other people.
This usually happens when there is close or long contact with a sick person in the same household or day care centre, or if they had direct contact with a patient’s oral secretions (such as a boyfriend or girlfriend). People who qualify as close contacts of a person with meningococcal or Haemophilus influenzae type b (Hib) meningitis are at higher risk of getting disease and may need preventive antibiotics .
Close contacts of a person with meningitis caused by other bacteria, such as Streptococcus pneumoniae, do not need antibiotics. Tell your doctor if you think you have been exposed to someone with meningitis. Healthy people can carry the bacteria in their nose or throat without getting sick. Rarely, these bacteria can invade the body and cause disease. Most people who ‘‘carry’’ the bacteria never become sick.
Signs and Symptoms
Meningitis infection may show up in a person by a sudden onset of fever, headache, and stiff neck. It will often have other symptoms, such as: Nausea, vomiting, increased sensitivity to light (photophobia), and altered mental status (confusion).
The symptoms of bacterial meningitis can appear quickly or over several days. Typically they develop within 3-7 days after exposure. Babies younger than one month old are at a higher risk for severe infections, like meningitis, than older children. In new-borns and infants, the classic meningitis symptoms of fever, headache, and neck stiffness may be absent or difficult to notice. The infant may appear to be slow or inactive (lack of alertness), irritable, vomiting or feeding poorly. In young infants, doctors may look for a bulging fontanelle (soft spot on infant’s head) or abnormal reflexes, which can also be signs of meningitis. If you think your infant has any of these symptoms, call the doctor or clinic right away. Later symptoms of bacterial meningitis can be very severe (eg, seizures, coma). For this reason, anyone who thinks they may have meningitis should see a doctor as soon as possible.
Diagnosis
If meningitis is suspected, samples of blood or cerebrospinal fluid (near the spinal cord) are collected and sent to the laboratory for testing. It is important to know the specific cause of meningitis because that helps doctors understand how to treat the disease, and possibly how bad it will get. In the case of bacterial meningitis, antibiotics can help prevent severe illness and reduce the spread of infection from person to person (depending on which bacteria are causing the infection).
If bacteria are present, they can often be grown (cultured). Growing the bacteria in the laboratory is important for confirming the presence of bacteria, identifying the specific type of bacteria that is causing the infection, and deciding which antibiotic will work best. Other tests can sometimes find and identify the bacteria if the cultures do not.
Treatment
Bacterial meningitis can be treated effectively with antibiotics. It is important that treatment be started as soon as possible. Appropriate antibiotic treatment of the most common types of bacterial meningitis should reduce the risk of dying from meningitis to below 15 percent, although the risk remains higher among young infants and the elderly.
Prevention
The most effective way to protect you and your child against certain types of bacterial meningitis is to complete the recommended vaccine schedule. Antibiotics may be recommended for close contacts of people with meningococcal meningitis. Antibiotics may also be recommended for the entire family if a family member develops severe Hib infection and there’s a high-risk person in the house. This is to decrease the risk of spreading disease to that person, since they are at increased risk for severe disease.
Your doctor or local health department will tell you if there’s a high-risk person in your house and whether antibiotics are needed. Maintaining healthy habits, like not smoking and avoiding cigarette smoke, getting plenty of rest, and not coming into close contact with people who are sick, can also help. This is especially important for young infants, the elderly, and people with a weakened immune system, since they are at increased risk for severe disease.
Meningitis is a very wide topic and I would advice those that like to know more to email me at [email protected].
Visit my blog www.healthpromotionbyleeanne.wordpress.com or read articles posted by the World Health Organisation.
‘‘Take care of your busy body, you owe that to your family.’’
Lee-Anne Hall, BSc Physiotherapy



